Originally published by The Ophthalmologist
Introducing iCare ST500, the world’s first slit-lamp-mounted rebound tonometer
While tonometry is routinely performed using a Goldmann applanation tonometer (GAT), disadvantages with the device have been documented in recent years. For example, GAT’s use of reusable prisms means that infection transmission becomes a possibility if the prisms are not disinfected properly, particularly for epidemic keratoconjunctivitis (1). Calibration issues have also been noted with the GAT units, which require regular calibration and are prone to drift, resulting in miscalibrations and systematic errors when this goes unnoticed in busy clinics (2). Given GAT measurements can also be partly subjective and depend on the skill of the operator for accuracy, there have also been recorded issues with operator bias potential in the device (3).
Streamlining workflow
iCare ST500™, the world’s first slit-lamp-mounted rebound tonometer, is a perfect addition to an ophthalmologist’s armamentarium, particularly for those looking to streamline their intraocular pressure (IOP) assessments and address these common GAT concerns. For glaucoma specialists or general ophthalmologists running high-throughput clinics, iCare ST500 offers time savings, less patient prep, and more seamless incorporation of IOP checks into the slit-lamp exam.
“I had been familiar with rebound tonometry for years and appreciated its comfort and speed. When a version appeared that could be mounted directly on the slit lamp, it immediately filled a practical gap in our clinic,” explains Dr. Francesco Oddone, Head of the Glaucoma Unit at the Britannic Hospital of the IRCCS Fondazione Bietti in Rome. “Most of our examination time happens at the slit lamp, so bringing IOP measurement to that exact point streamlines the visit.”
Because iCare ST500 mounts via a universal adaptor compatible with most slit lamps, it allows ophthalmologists to incorporate their IOP measurements into the standard slit lamp exam without the need for changing devices.
“The fact that it lives on the slit lamp is key,” adds Dr Oddone. “We can measure IOP before or during the anterior segment evaluation, without instilling drops or moving the patient. Technicians can capture pressures independently and consistently, which makes the physician’s time at the scope more efficient. And because there’s no prism to disinfect, we’ve removed a common bottleneck between patients. The overall effect is a more predictable, interchangeable workflow across operators, with fewer interruptions for drop instillation and a simpler path to repeat a measurement if something looks borderline.”
Rebound revolution
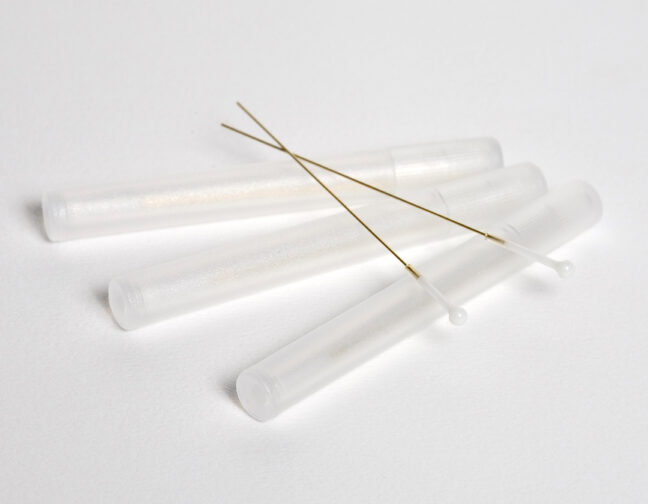
Relying less on the manual IOP measurements of GAT, rebound tonometry measures IOP by firing a very small probe toward the cornea and analyzing its motion as it contacts and rebounds.
Dr. Oddone explains the measurement mechanics in greater detail: “The underlying physics is elegant: a lightweight probe touches and rebounds from the cornea, and the device infers the pressure by analyzing the rebound deceleration and time before converting this into millimeters of mercury. The instrument takes multiple micro-measurements in a short burst and discards outliers automatically, then displays an average with a quality indicator that tells you whether to accept the result or repeat it. Because the probe mass and travel are so carefully engineered, patients perceive at most a soft tap, which explains the excellent tolerability and the repeatability we see in routine use.”
The disposable probe touches the cornea for only the briefest, gentlest moment, making the measurement almost imperceptible to the patient, and requiring no anesthetic drops and no fluorescein dye.
“Patients tolerate the brief contact extremely well, with very little squeezing or flinching,” notes Dr. Oddone. “The absence of anesthetic and fluorescein is immediately noticeable to patients, particularly those with ocular surface disease or heightened anxiety,” he adds. “Because the measurement happens within the biomicroscopy flow, it becomes natural to perform situational checks, for example before gonioscopy or after dilation, when you might otherwise forgo an extra IOP reading.”
A viable alternative to GAT?
Utilizing iCare’s patented rebound algorithm, iCare ST500 does not require daily user calibration, simplifying workflow and addressing the aforementioned GAT concerns over potential miscalibrations (2) and operator bias (3).
“Compared with Goldmann applanation, iCare ST500 removes the need for anesthetic and fluorescein, which speeds up the visit and avoids tear-film staining that can complicate subsequent observations,” explains Dr. Oddone. “Hygiene is simpler because there are no prisms to disinfect or maintain, and you avoid the subtle biases that can creep in when reading mires. There’s also no prism wear to worry about, which reduces the risk of drift from surface imperfections over time.”
Dr. Oddone goes on to explain that during the iCare ST500 adoption phase, his team ran paired measurements, iCare ST500 followed by GAT, to reassure themselves that agreement was uniform in their own patient mix. “The results were consistently coherent,” he says. “When differences arose, they typically reflected factors we already interpret carefully, such as corneal biomechanics or surface irregularities. That internal, real-world cross-check gave us the confidence to make iCare ST500 our routine first measure, and to use Goldmann selectively for confirmation in specific scenarios.”
For particularly uncooperative patients, iCare ST500 also offers a “Quick Measure” mode, which allows for two or three rapid readings instead of the typical six. This can be especially helpful when dealing with patients who struggle with fixation or blinking.
“Quick Measure comes into its own when perfect alignment or multiple cycles aren’t feasible – e.g., in children, patients with blepharospasm or tremor, or anyone who is particularly anxious,” says Dr. Oddone. “A gentle stabilization and a broad alignment are often enough to capture a rapid sequence that yields a clinically actionable number. In those situations, it’s not just a convenience; it can be the difference between obtaining useful data and having no measurement at all.”
Pragmatic advances
In Dr. Oddone’s own practice in Rome, the team have now adopted iCare ST500 as their default initial IOP measuring device, adding Goldmann only when it is indicated by the clinical context.
“The goal is a lean, reproducible pathway: reliable pressures captured quickly, with confirmatory steps reserved for the cases that truly need them,” he says. “iCare ST500 already functions as a pragmatic standard. It is faster, cleaner, very well accepted by patients, and accurate enough for the vast majority of clinical decisions. As clinics continue to prioritize efficiency and infection control, and as teams standardize around digital outputs, I expect its role to keep expanding while GAT is used more selectively rather than by default.”
For successful glaucoma specialists like Dr. Oddone who are seeking to modernize and streamline IOP measurements in their high-volume clinics, iCare ST500 represents a meaningful advancement in tonometry, one that provides less patient prep, better integration, and an enhancement of both clinical efficiency and patient experience.
References
- J Massey et al., “Notes from the Field: Health Care-Associated Outbreak of Epidemic Keratoconjunctivitis–West Virginia, 2015,” MMWR Morb Mortal Wkly Rep, 65, 382 (2016). PMID: 27078721.
- JY Chuo, FS Mikelberg, “Calibration errors of Goldmann tonometers in a tertiary eye care centre,” Can J Ophthalmol., 42, 712 (2007). PMID: 17891198.
- I Mostafa et al., “What is the best way to measure intraocular pressure (IOP) in a virtual clinic?,” Eye (Lond)., 35, 448 (2020). PMID: 32322017.